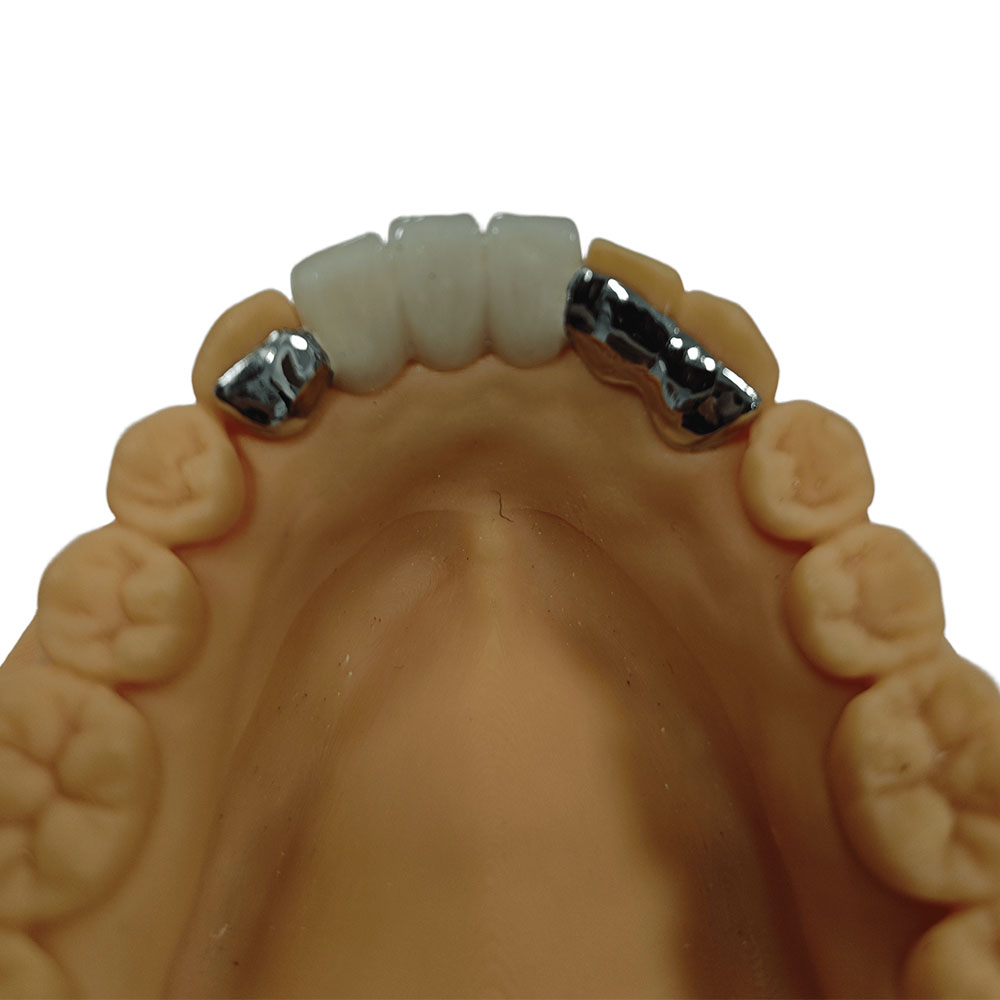
PFM
Istar Dental Lab, a leading Chinese manufacturer, provides precision-crafted PFM crowns and bridges. We combine advanced CAD/CAM technology with premium, biocompatible materials for natural aesthetics and long-lasting strength. Experience reliable, cost-effective solutions, consistent quality, and dedicated technical support. Optimize your workflow and patient satisfaction with Istar.
PFM Crowns and Bridges
Porcelain Fused to Metal (PFM) restorations, which include crowns and fixed dental prostheses (FDPs or bridges), are a better choice than older options. They are an improvement over full gold crowns, which were strong but didn’t look natural, and early porcelain jackets, which looked nice but broke easily. PFMs have been a key part of fixing teeth and have been a dependable treatment option for more than 50 years. Our ceramic/porcelain fused to metal crowns and bridges use top-quality materials and fit very well in the mouth.
What Is a PFM Crown and Bridge Made of?
A ceramic/porcelain fused to metal crown and bridge is made of two parts:
- Metal Base: This part is strong. It goes on your tooth and keeps the crown or bridge in place.
- Porcelain Layer: This part covers the metal and matches the color of your real teeth.
Why Choose PFM Crowns and Bridges?
PFM crowns and bridges are popular all over the world. Here’s why:
- Stærk og langtidsholdbar: The metal makes them very tough.
- Se naturlig ud: The porcelain is colored to look like your teeth.
- Fits Many Needs: Can fix one tooth or many missing teeth.
- Safe Materials: Uses special metals that are safe for your mouth.
- Proven Track Record: Dentists have trusted ceramic/porcelain fused to metal crowns and bridges for decades.
Who Uses PFM Dental Crown and Bridge?
When PFM Restorations are a Good Idea:
- When a tooth is too damaged for a simple filling.
- When a tooth needs to be fully covered for strength and to keep it safe.
- To support fixed dental prostheses (bridges), especially long ones.
- For teeth that handle a lot of chewing pressure.
- In places with limited space between teeth where a strong but thin base is needed.
- For patients who grind their teeth (bruxism) and need something very strong that won’t break.
- When cost is a concern and all-ceramic options are too expensive.
When PFM Restorations are NOT a Good Idea:
- For patients with known allergies to metals (like nickel).
- When a perfect look is needed for front teeth, where the dark metal might show through, especially if the gums are thin (thin gingival biotypes).
- For patients who want restorations that have no metal at all.
- When there isn’t enough of the natural tooth left to hold the crown securely.
- If there is active gum disease or cavities that haven’t been treated.
What Are They Made Of?
PFM alloys are grouped by how much noble metal they contain:
- Højadelige legeringer: Have ≥60% noble metals (gold, platinum, palladium) and at least 40% gold. Au-Pt-Pd alloys are one example. Small amounts of elements like Indium (In), Tin (Sn), and Iron (Fe) are often added to help create the right kind of oxide layer so the porcelain sticks better.
- Noble Alloys: Have ≥25% noble metals. Pd-Ag and Pd-Cu alloys are examples. These create thinner, less reactive oxide layers. They act in a way that’s in between the other two types. Palladium (Pd) helps the oxide form, but Silver (Ag) can sometimes stain the porcelain or make the bond weak if not handled very carefully.
- Base Metal Alloys: Have <25% noble metals. Ni-Cr and Co-Cr alloys are examples. These alloys make thicker, more reactive oxide layers (like Cr₂O₃). This helps the porcelain bond chemically, but there’s a risk that too much oxide can grow, making the connection point brittle.
Each type has different qualities that affect how well the porcelain bonds, how easy it is to cast, and how safe it is for the body.
How the Lab Makes PFM Restorations
Making PFM restorations in a lab is a detailed process with many steps that requires careful work, knowledge of materials, and an artistic touch. Many dental labs now use digital tools to make the process faster and more accurate.
Model Work and Die Preparation
After getting molds (either physical molds or digital scans), the lab starts by making the model.
Making the Metal Framework
The metal framework (called a coping or substructure) gives the restoration its strength and support. There are two main ways to make it: the traditional lost-wax casting method and using CAD/CAM to mill the framework.
Layering the Porcelain
After the metal framework is ready, the detailed and skillful process of adding the porcelain layers starts. This requires a lot of artistic and technical ability.
Careful Firing Schedules
Each layer of porcelain is heated in a special furnace using exact temperature and vacuum schedules.
Final Finishing and Glazing
After all the porcelain layers are put on and fired, they need to be shaped, adjusted, glazed (to give them a shiny, smooth surface), and polished.
Product Specifications Table
Here is a simple table with the main details about our PFM dental crowns and bridges:
| Funktion | Detaljer |
|---|---|
| Type | PFM crowns and bridges; ceramic/porcelain fused to metal crowns and bridges |
| Materiale | Metal alloy (high-noble, noble, or base) + porcelain layer |
| Valgmuligheder i metal | Gold, Palladium, Titanium, Cobalt-Chromium, Nickel-free, Beryllium-free |
| Porcelæn | Custom shade matched, strong, looks like a real tooth |
| Dækning | Full crown, Multi-unit bridge, Single tooth, Pontic |
| Teknik | CAD/CAM or traditional lab process |
| Pasform | Very precise, tight edge |
| Size Range | Single crowns, bridges up to 14 teeth |
| Farvemuligheder | Full range of shades, looks naturally see-through |
| Levetid | 10-15 years on average, longer with good care |
| Indications | Decayed teeth, broken teeth, missing teeth, after root canals |
| Cementering | Standard dental cements |
| Requirement | Tooth needs to be shaped down, with proper edges (shoulder or chamfer) |
Our Thorough Quality Control Checks
We use strict quality control (QC) during every step of making and delivering PFM restorations to make sure they fit, work, and look perfect.
- Model and Die Accuracy: Checking that the mold is accurate and the model is solid.
- Framework Fit: Carefully checking the metal framework on the model to see that the edges are sealed, it fits on the inside, and it sits down correctly.
- Porcelain Layering: Looking closely to see that the porcelain is an even thickness, has no tiny holes, and is the right color.
- Firing Check: Watching the firing process and looking for any cracks, tiny surface fractures, or separation of layers.
- Bite and Side Contacts: Making sure the bite is correct and the contacts between teeth are tight on the model.
- Appearance Check: Judging the color, translucency, surface texture, and overall look under special lights.
- Color Difference Checks: We regularly measure color differences (ΔE₀₀, ΔEₐₑ). A ΔE₀₀ value below 1.8 is usually not noticeable, while values up to 3.3 are acceptable for PFM restorations in a patient’s mouth.
Long-Term Success Rates of Our PFM Crowns and Bridges
Many scientific studies have shown that PFM restorations have very good survival rates:
- 10-year survival rates:
- PFM crowns: 85–95%
- PFM fixed dental prostheses (bridges): 80–90%
- 15-year survival rates:
- PFM bridges: Drop to 70–80%
- Single crowns: Usually have slightly higher rates.
These numbers show how strong and dependable PFM restorations are, especially in areas that take a lot of chewing force.
How Do Dentists Use PFM Crowns and Bridges?
Preparing the tooth correctly is the most important step for making sure a PFM restoration works well and looks good.
Tooth Reduction Guidelines:
- Bite Surface Reduction: For back teeth that take a lot of chewing force, 1.5–2.0 mm of the chewing surface should be removed. This makes sure there is enough material for both the metal base (at least 0.5 mm) and the porcelain cover (at least 1.0–1.5 mm), which greatly lowers the chance of the porcelain breaking. For patients who grind their teeth, removing up to 2.0 mm and using stronger metals is a good idea.
- Side Reduction: The sides of the tooth should be reduced by 1.2–1.5 mm in areas you can see (like front teeth) and 1.0–1.2 mm for back teeth. This leaves enough room for the metal and porcelain layers.
- Minimum Metal Thickness: High-noble alloys can be made a bit thinner (0.3–0.5 mm) because they have better strength and flexibility. Base metal alloys need to be at least 0.5 mm thick to be strong enough and not bend under chewing pressure.
Finish Line Design:
- Shoulder or Deep Chamfer: When looks are very important (like on front teeth or visible edges), a shoulder or deep chamfer finish line (1.0–1.2 mm) is suggested. This design leaves enough room for the right thickness of porcelain, which helps it look natural and have the right color, especially if a porcelain edge is used.
- Light Chamfer: A light chamfer (0.5–0.7 mm) can be used for standard metal edges, but this might not look as good if the metal edge can be seen.
- Edge Fit: Studies (like Sulaiman et al., 2021) show that shoulder and deep chamfer finish lines provide a better fit at the edge (<50 μm gap) than feather-edge or knife-edge designs. This is linked to fewer new cavities and less gum irritation. The fit of the edge also depends on the metal used; base metal alloys change shape less during porcelain firing than high-noble alloys.
Taper and Retention:
- A recommended taper of 6–12° is needed to help the crown stay on and resist being pulled off. If the taper is too wide (>20°), the crown won’t stay on as well, especially on short teeth.
Fracture Resistance:
- Even reduction and rounded inside corners are very important for preventing cracks by spreading out the chewing forces evenly. Not enough reduction or sharp inside corners greatly increases the risk of the porcelain chipping or breaking completely.
How it Affects the Tooth and Bite:
- Removing too much tooth structure increases the risk of damaging the nerve and causing pain after the procedure. On the other hand, not removing enough tooth makes the restoration weaker and look worse.
- Finite Element Analysis (FEA) studies (like Zhang et al., 2022) show that deep chamfer and shoulder designs spread chewing forces out in a better way, which reduces stress on the rest of the tooth.
Impression Methods
- Traditional Impressions: Polyvinyl siloxane (PVS) or polyether materials are typically used. Careful technique, including moving the gum tissue away from the tooth and using the right tray, is very important to get all the details of the prepared tooth, especially the finish line.
- Digital Scanning: Intraoral scanners (like 3Shape TRIOS, iTero, Medit i700) are a very accurate and fast alternative. Recent studies (like Lee et al., 2023) show that digital impressions produce gaps at the edge that are as small as, or smaller than, those from traditional PVS impressions, with average gaps of 30–60 μm. Digital methods reduce human error and allow for a more exact design of the finish line, especially in areas below the gumline.
Temporary Crown Strategies
- Temporary crowns are needed to protect the prepared tooth, keep the bite the same, and keep the gums healthy.
- Temporary crowns should fit well at the edges, have the right shape where they meet the gums, and be made of strong enough materials (like bis-acryl composites).
- The goal is to stop leaks and prevent irritation of the gums, aiming for a Gingival Index of <1.0 while the temporary is in place.
- Using spot-etching or temporary cements without eugenol (like TempBond NE) is suggested to not interfere with the final cement and to keep the gums healthy.
Final Cementing Steps
- Keeping it Dry: It’s very important to keep the area dry (for example, with a rubber dam) to prevent it from getting contaminated.
- Rengøring: The inside of the PFM crown and the prepared tooth must be cleaned completely.
- Choosing a Cement: Resin-modified glass ionomer cements (RMGICs) or resin cements are often used because they have a strong bond, don’t dissolve easily, and release fluoride. For high-noble alloys, traditional glass ionomer cements or zinc phosphate cements can also work well.
- Seating and Curing: The restoration must be pushed down fully with firm, steady pressure. Extra cement must be carefully removed, especially from the space around the gum, to prevent gum inflammation. If using a resin cement, follow the manufacturer’s instructions for light-curing.
Brugsscenarier
PFMs are still a very important and necessary choice for certain clinical situations, including:
- Long-span bridges: Their natural strength and stiffness make them a great choice for restorations with multiple teeth where all-ceramics might break.
- Cases with limited chewing space: They are useful because they can be made strong even when the metal base is thin, compared to some all-ceramic materials.
- Situations needing high fracture resistance: PFMs have a long history of being strong and durable, especially for back teeth or in patients who grind their teeth.
Easy Care Instructions
It’s very important for patients to follow care instructions to make their PFM restorations last as long as possible.
- Oral Hygiene: Careful daily cleaning, including brushing with a soft-bristled toothbrush and non-gritty toothpaste, and flossing, is necessary to prevent plaque buildup, new cavities, and gum inflammation around the edges of the restoration.
- Dietary Habits: Patients should be told to avoid chewing on very hard things (like ice or hard candies) that could chip the porcelain. If a restoration has been repaired, it’s a good idea to avoid hard foods for at least 48 hours after the repair.
- Occlusal Guards: For patients who grind or clench their teeth, using a custom-made occlusal guard (nightguard) is highly recommended to protect the PFM restoration from too much chewing force and to prevent the porcelain from chipping or breaking.
- Regular Dental Check-ups: Seeing a dentist twice a year is key for finding any problems early (like gaps at the edges, chipped porcelain, new cavities, or changes in the gums) and fixing them quickly.
- Avoidance of Whitening Agents: Patients should know that whitening products will not change the color of the PFM restoration, and using them might make their natural teeth a different color than the crown.
By following these complete repair and care plans, dentists and labs can greatly increase the usable and cosmetic life of PFM restorations, giving patients long-term value and happiness.