How Do Dentists Treat an Infected Tooth? A Calm, Honest Guide from “Uh-oh” to “All Good”
An infected tooth isn’t just a “bad tooth.” It’s your body sending a very serious, very fixable signal. This guide walks you through exactly what dentists actually do—from the moment you sit in the chair to the moment you can bite, sleep, and smile like yourself again.
No fluff, no scare tactics, no miracle hacks. Just a human, clear, deeply thought-through breakdown designed to beat generic dental blogs on depth, empathy, and accuracy.
Table of Contents
1. First: what does “infected tooth” really mean?
When dentists talk about an infected tooth, they’re usually referring to:
- infection inside the tooth (the pulp and root)
- infection at the tip of the root (periapical abscess)
- or infection in the gums around the tooth (periodontal abscess)
In all cases, the core problem is bacteria breaking through enamel/dentin, reaching tissue that really doesn’t like being invaded. Left alone, that infection can spread to your jaw, face, airway, or bloodstream—which is why real dental treatment is non-negotiable. Authoritative medical sources are very clear: antibiotics alone are not a cure; the source tooth must be treated.
- Common signals you’re dealing with an infection:
- Throbbing toothache that may pulse with your heartbeat
- Swelling in the gum, cheek, or jaw
- Pimple-like bump on the gum that may ooze
- Pain when biting or tapping the tooth
- Bad taste or breath that won’t go away
- Fever, feeling run down (red flag: systemic spread)
2. How dentists decide what your tooth actually needs
Before anyone drills, drains, or extracts, your dentist’s first job is detective work.
They will usually:
- listen to your story (onset, triggers, past dental work)
- examine your tooth and gums visually
- tap, press, and temperature-test the tooth
- take X-rays to see the root, bone, and any hidden abscess
- consider your medical history (diabetes, heart disease, pregnancy, meds, etc.)
All of this is to answer one question:
“Can we safely save this tooth—or is removing it the healthiest move for your whole body?”
- What this means for you in the chair:
- Expect questions; honest answers shape safer treatment
- Expect X-rays; they are not “upsells,” they’re the map
- Expect a clear explanation of: what’s infected, how badly, and what options exist
3. Step One in Treatment: calm the infection, calm the pain
Here’s the part most people misunderstand: treating an infected tooth is about removing the source, not just killing stray bacteria.
At this early stage your dentist may:
- Open and drain the infection
- If there’s a visible abscess, they might numb the area, make a tiny opening, and let the pus drain. Instant pressure relief.
- Start definitive tooth treatment (often the same visit)
- Begin a root canal or other procedure to clean out infected tissue.
- Prescribe antibiotics—only when indicated
- Used if the infection is spreading (swelling, fever, difficulty swallowing/closing mouth) or you’re medically vulnerable. On their own, they do not “fix” the tooth; they just support your body while the real treatment happens.
- You might notice your dentist:
- Prioritizing drainage + cleaning over “just giving antibiotics”
- Talking urgently if there’s facial swelling, fever, or trouble breathing (this is not drama; it’s safety)
- Reassuring you that numbing will be thorough before any procedure

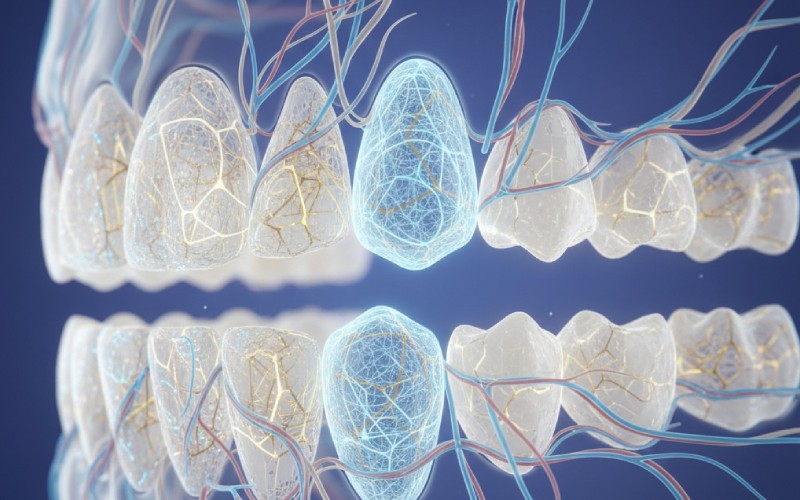
4. Root canal: the hero treatment that (quietly) saves your tooth
If the tooth structure is still solid and the infection is inside the pulp/root, a root canal is usually the gold-standard.
In human terms, a root canal is:
“We keep the shell of your tooth, remove the angry infected nerve, disinfect the inside, and seal it so bacteria can’t make it their Airbnb again.”
Key steps (simplified):
- numb the tooth (this is usually the most “dramatic” part; after that, you mostly feel pressure, not pain)
- make a small opening on top
- remove infected pulp and bacteria from the canals
- rinse with disinfectant solutions
- fill canals tightly with a bio-safe material
- often place a crown after to protect the weakened tooth long-term
- Emotionally & practically, here’s what to know:
- Modern root canals are nothing like horror stories; they’re closer to a long filling
- They’re designed to end pain, not cause it
- When done well and crowned, that tooth can last many years
5. At-a-glance: how dentists treat an infected tooth (comparison table)
| Treatment Option | Best For | What Happens | Sensation (With Numbing) | Big Picture Outcome |
|---|---|---|---|---|
| Drainage of abscess | Localized swelling, pus pocket | Small incision, pus released, area cleaned | Brief pressure, quick relief | Buys comfort; usually needs further tx |
| Root canal | Infected pulp, tooth still savable | Pulp removed, canals cleaned & filled, crown | Pressure/vibration, not sharp | Saves tooth, removes infection source |
| Pulpotomy / pulpectomy | Often in kids’ teeth, early/mid infection | Part/whole pulp removed, tooth sealed | Similar to filling | Preserves tooth until natural shedding |
| Gum / periodontal therapy | Infection from deep gum pockets | Deep cleaning, possible surgery, drainage | Numbed; scraping/pressure | Treats gum cause, saves surrounding bone |
| Extraction | Tooth cracked, unsalvageable, severe damage | Tooth removed, abscess drained | Pressure, no pain with good LA | Removes problem; can replace tooth |
| Antibiotics | Spreading infection, systemic risks | Oral/IV medication alongside dental procedure | No procedure feel | Supports healing; never solo cure |
6. When is extraction the wiser, kinder choice?
No ethical dentist wants to pull a tooth that can be saved. But there are times removal is genuinely in your best interest:
- the tooth is split/cracked below the gum
- there’s massive decay with not enough tooth left to rebuild
- repeated failed root canal or severe re-infection
- advanced bone loss around the tooth
In those cases, extraction:
- stops the infection at its source
- lets surrounding bone and tissue heal
- opens the door to replacements (implant, bridge, partial denture)
- Your dentist should walk you through:
- why they think the tooth can’t be saved
- what replacement options fit your age, bite, budget, and health
- what healing will look like day-by-day (pain, swelling, normal vs not)

7. What if the infection is in the gums, not just the tooth?
Sometimes the infection is mainly in the supporting tissues—this is a periodontal abscess.
Treatment often includes:
- draining the abscess through the gum
- deep cleaning (scaling and root planing) to remove plaque and tartar
- treating underlying gum disease
- sometimes minor surgery to access and clean deeper areas
- antibiotics in selected cases
- How this feels from your side:
- You may hear about “deep cleaning”—that’s medical, not cosmetic
- The dentist will emphasize long-term gum care, not one-time fixes
- You’ll be a co-pilot here: without your home care, it just comes back
8. Myths your dentist secretly hopes you’ll stop believing
Let’s quickly dismantle a few ideas that keep infections worse for longer:
- “If the pain went away, the infection is gone.” Often the nerve died. Infection can silently spread.
- “I’ll just get antibiotics over the counter.” Even if you could, it’s incomplete care and promotes resistance.
- “Root canals are torture; extraction is easier.” A well-done root canal is controlled, predictable relief—and you keep your tooth.
- “I can pop the abscess myself.” That’s a fast track to spreading bacteria into deeper spaces. Dentists use sterile technique for a reason.
- Healthier truths to keep instead:
- Pain relief ≠ infection cured
- Any facial swelling, fever, or trouble swallowing = urgent same-day care
- Treating early = less cost, less drama, more tooth
9. Red flag signs: when a tooth infection is an emergency
A tooth infection can, in rare cases, become life-threatening. You should seek urgent or emergency care if you notice:
- swelling spreading to eye, neck, or floor of the mouth
- difficulty swallowing, speaking, or opening your mouth
- fever + feeling very unwell or confused
- drooling because it hurts to swallow
- trouble breathing or noisy breathing
At that point, it’s not “just a toothache”; it’s an airway and systemic issue. You may need hospital-based drainage and IV antibiotics alongside dental treatment.
- Simple rule: If your face shape changes or basic functions (breathing, swallowing, opening mouth) are affected, treat it as an emergency, not a Monday problem.
10. Healing: what a “good” recovery usually looks like
After proper treatment, most people experience:
- pain shifting from sharp/throbbing → mild soreness
- swelling gradually shrinking over 24–72 hours
- better sleep, easier chewing on the other side initially
- follow-up visit to confirm healing (and place a crown, if needed)
- Your part in recovery (what actually helps):
- Take prescribed meds as directed (finish antibiotics if given)
- Don’t smoke or vape; it slows healing
- Keep the area clean according to your dentist’s instructions
- Call if pain worsens after initially improving, or new swelling/fever appears
11. How to not end up here again
Once you’ve stared down an infected tooth, preventing the sequel is smart, not “fussy.”
Daily choices that genuinely lower your risk:
- brushing twice daily with fluoride toothpaste
- cleaning between teeth (floss, interdental brushes, or water flosser)
- not ignoring small chips, sensitivity, or food-trap areas
- regular check-ups + X-rays so decay is caught early
- managing dry mouth, diabetes, and smoking if they apply to you
- Think of it this way:
- Infections love hidden, forgotten corners
- Your future self will never complain about the appointment you kept early
12. A quick FAQ
“Will it hurt?” During treatment, you should feel pressure, not sharp pain. If you do, your dentist can give more anesthetic. You are allowed to speak up.
“Can I ask for step-by-step explanations?” Please do. A good dentist will tell you what’s coming next, show you X-rays, and translate jargon into normal language.
“Is it ever okay to ‘wait and see’ with an infected tooth?” If there’s true infection (abscess, swelling, severe lingering pain), waiting doesn’t make it heal; it only gives bacteria more space.
“What’s the single most important thing to remember?” Treat the source of the infection, not just the symptoms. Every responsible dental plan is built around that idea.